Sunscreen
Sunscreen (also known as sunblock, suntan lotion) is a lotion, spray or other topical product that helps protect the skin from the sun's ultraviolet (UV) radiation, and which reduces sunburn and other skin damage, ultimately leading to a lower risk of skin cancer. However, suntan lotion is an incorrect term for sunscreen as it is something entirely different. Suntan lotion is used to attract UV rays in order to better tan where sunblock is used to deflect UV radiation. These are commonly called indoor tanning lotions when designed for use with tanning beds or just suntan lotion if designed for outdoor use and may or may not have SPF protection in them.
The best sunscreens protect against both UVB (ultraviolet radiation with wavelength between 290 and 320 nanometres), which can cause sunburn, and UVA (between 320 and 400 nanometres), which damages the skin with more long-term effects, such as premature skin aging. Most sunscreens work by containing either an organic chemical compound that absorbs ultraviolet light (such as oxybenzone) or an opaque material that reflects light (such as titanium dioxide, zinc oxide), or a combination of both. Typically, absorptive materials are referred to as chemical blocks, whereas opaque materials are mineral or physical blocks.
Dosing for sunscreen can be calculated using the formula for body surface area and subsequently subtracting the area covered by clothing that provides effective UV protection. The dose used in FDA sunscreen testing is 2 mg/cm².[1] Provided one assumes an "average" adult build of height 5 ft 4 in (163 cm) and weight 150 lb (68 kg) with a 32 in (82 cm) waist, that adult wearing a bathing suit covering the groin area should apply 29 g (approximately 1 oz) evenly to the uncovered body area. Considering only the face, this translates to about 1/4 to 1/3 of a teaspoon for the average adult face.
Contrary to the common advice that sunscreen should be reapplied every 2–3 hours, research has shown that the best protection is achieved by application 15–30 minutes before exposure, followed by one reapplication 15–30 minutes after the sun exposure begins. Further reapplication is only necessary after activities such as swimming, sweating, and rubbing.[2]
However, more recent research at the University of California indicates that sunscreen needs to be reapplied within 2 hours in order to remain effective. Not reapplying could even cause more cell damage than not using sunscreen at all, due to the release of extra free radicals from absorbed chemicals.[3]
A significant reduction in sun exposure inhibits the production of vitamin D. The use of sunscreen with a sun protection factor (SPF) of 8 inhibits more than 95% of vitamin D production in the skin.[4] However, excessive sun exposure has been conclusively linked to some forms of skin cancer and signs of premature aging. Season, geographic latitude, time of day, cloud cover, smog, skin type, and sunscreen all have an effect on vitamin D production in the skin.[5] Fifteen minutes per day of direct exposure to the sun (i.e. without sunscreen) is a generally accepted guideline to follow for optimum vitamin D production.[6]
History
The ancient Greeks used olive oil as a type of sunscreen. However, this was not very effective. Throughout the early twentieth century, H.A. Milton Blake, a South Australian chemist, as well as several other inventors attempted to create an effective sunscreen but failed.
It was not until 1944 that the first effective sunscreen was invented. At that time, World War II was in full swing and many soldiers were getting serious sunburn. A pharmacist named Benjamin Greene decided to create something that would save the soldiers from the sun’s harmful rays. In his wife’s oven, he created a sticky, red substance which he called "red vet pet" (red veterinary petrolatum), which worked primarily by physically blocking the sun's rays with a thick petroleum-based product similar to Vaseline. Greene tested it on his own bald head. It did not work nearly as well as modern sunscreens, but it was a start.
Sunscreen has come a long way since its initial days. Modern products have much higher protection factors than Greene's sunscreen, and modern products can also be water- and sweat-resistant. But there are also negative effects. Some people rely too much on the product and do not understand the limitations of the sun protection factor (SPF); they assume that buying anything over SPF 30 will automatically prevent them getting burnt no matter how long they can stay in the sun. Too much sunbathing is one of the major causes of skin cancer across the world.
An effective sunscreen had already been developed in 1938 by the Swiss chemistry student Franz Greiter, after he had severely burnt himself during an ascent of the Piz Buin on the border between Switzerland and Austria. He named his product, which he had developed in a small laboratory in his parents' home, Gletscher Creme or in English Glacier Cream. Still existing examples of the 'Glacier Cream' have shown to have a SPF of 2 and thus could be classed as an effective sunscreen.
Mechanism of action
The principal ingredients in sunscreens are usually aromatic molecules conjugated with carbonyl groups. This general structure allows the molecule to absorb high-energy ultraviolet rays and release the energy as lower-energy rays, thereby preventing the skin-damaging ultraviolet rays from reaching the skin. So, upon exposure to UV light, most of the ingredients (with the notable exception of avobenzone) do not undergo significant chemical change, allowing these ingredients to retain the UV-absorbing potency without significant photo-degradation.[1]
Measurements of Sunscreen Protection
Sun protection factor
The SPF (sun protection factor) of a sunscreen is a laboratory measure of the effectiveness of sunscreen; the higher the SPF, the more protection a sunscreen offers against UV-B (the ultraviolet radiation that causes sunburn). The SPF indicates the time a person can be exposed to sunlight before getting sunburn with a sunscreen applied relative to the time they can be exposed without sunscreen. For example, someone who would burn after 12 minutes in the sun would expect to burn after 2 hours (120 min) if protected by a sunscreen with SPF 10. In practice, the protection from a particular sunscreen depends on factors such as:
- The skin type of the user.
- The amount applied and frequency of re-application.
- Activities in which one engages (for example, swimming leads to a loss of sunscreen from the skin).
- Amount of sunscreen the skin has absorbed.
The SPF is an imperfect measure of skin damage because invisible damage and skin aging is also caused by the very common ultraviolet type A, which does not cause reddening or pain. Conventional sunscreen does not block UVA as effectively as UVB, and an SPF rating of 30+ may translate to significantly lower levels of UVA protection according to a 2003 study. According to a 2004 study, UVA also causes DNA damage to cells deep within the skin, increasing the risk of malignant melanomas.[7] Even some products labeled "broad-spectrum UVA/UVB protection" do not provide good protection against UVA rays.[8] The best UVA protection is provided by products that contain zinc oxide, avobenzone and mexoryl. Titanium dioxide probably gives good protection, but does not completely cover the entire UV-A spectrum.[9]
Due to consumer confusion over the real degree and duration of protection offered, labeling restrictions are in force in several countries. In the United States in 1999, the Food and Drug Administration (FDA) decided to institute the labelling of SPF 30+ for sunscreens offering more protection, and a similar restriction applies in Australia. This was done to discourage companies from making unrealistic claims about the level of protection offered (such as "all day protection"),[10] and because an SPF over 30 does not provide significantly better protection. [11]
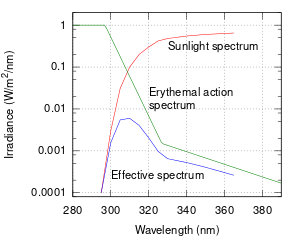
The SPF can be measured by applying sunscreen to the skin of a volunteer and measuring how long it takes before sunburn occurs when exposed to an artificial sunlight source. In the US, such an in vivo test is required by the FDA. It can also be measured in vitro with the help of a specially designed spectrometer. In this case, the actual transmittance of the sunscreen is measured, along with the degradation of the product due to being exposed to sunlight. In this case, the transmittance of the sunscreen must be measured over all wavelengths in the UV-B range (290–350 nm), along with a table of how effective various wavelengths are in causing sunburn (the erythemal action spectrum) and the actual intensity spectrum of sunlight (see the figure). Such in vitro measurements agree very well with in vivo measurements.[12]
Mathematically, the SPF is calculated from measured data as
- <math>\mathrm{SPF} = \frac{\int A(\lambda) E(\lambda)d\lambda}{\int A(\lambda) E(\lambda)/\mathrm{MPF}(\lambda) \, d\lambda},</math>
where <math>E(\lambda)</math> is the solar irradiance spectrum, <math>A(\lambda)</math> the erythemal action spectrum, and <math>\mathrm{MPF}(\lambda)</math> the monochromatic protection factor, all functions of the wavelength <math>\lambda</math>. The MPF is roughly the inverse of the transmittance at a given wavelength.
The above means that the SPF is not simply the inverse of the transmittance in the UV-B region. If that were true, then applying two layers of SPF 5 sunscreen would be equivalent to SPF 25 (5 times 5). The actual combined SPF is always lower than the square of the single-layer SPF.
The following are the FDA allowable active ingredients in sunblocks:
- p-Aminobenzoic acid (PABA) up to 15 %.
- Avobenzone up to 3%.
- Cinoxate up to 3%.
- Dioxybenzone up to 3%.
- Homosalate up to 15%.
- Menthyl anthranilate up to 5%.
- Octocrylene up to 10%.
- Octyl methoxycinnamate (Octinoxate) up to 7.5%.
- Octyl salicylate up to 5%.
- Oxybenzone up to 6%.
- Padimate O up to 8%.
- Phenylbenzimidazole sulfonic acid (Ensulizole) up to 4%.
- Sulisobenzone up to 10%.
- Titanium dioxide up to 25%.
- Trolamine salicylate up to 12 %.
- Zinc oxide up to 25%.
Others include:
- 4-Methylbenzylidene camphor (USAN Enzacamene)
- Tinosorb® M (USAN Bisoctrizole, INCI Methylene Bis-Benzotriazolyl Tetramethylbutylphenol)
- Tinosorb® S (USAN Bemotrizinol, INCI Bis-Ethylhexyloxyphenol Methoxyphenyl Triazine)
- Mexoryl® SX (USAN Ecamsule, INCI Terephthalylidene Dicamphor Sulfonic Acid)
- Mexoryl® XL (INCI Drometrizole Trisiloxane)
- Neo Heliopan® AP (INCI Disodium Phenyl Dibenzimidazole Tetrasulfonate)
- Uvinul® A Plus (INCI Diethylamino Hydroxybenzoyl Hexyl Benzoate)
- Uvinul® T 150 (INCI Octyl Triazone)
- Uvasorb® HEB (INCI Diethylhexyl Butamido Triazone)
- Parsol® SLX (INCI Polysilicone-15)
Most of these ingredients are not FDA approved, but all of them are approved within the EU. And some are permitted in other parts of the world as well. A lot of these relative new ingredients absorb UVA, making it easier for sunscreen manufacturers to formulate for the growing demand of sunscreens with better UVA protection.
Measurements of UVA Protection
Persistent Pigment Darkening (PPD), Immediate Pigment Darkening (IPD), Boots Star System, Japanese PA system
Star rating system
In the UK and Ireland, a star rating system is used to describe the ratio of UVA to UVB protection offered by sun screen creams and sprays. Invented by Dr Diffley of the Boots Company in Nottingham UK, it has been adopted by most companies marketing these products in the UK. It should not be confused with SPF which is measured with reference to burning and UVB. One star products provide the least ratio of UVA protection, five star products are the best.
Melanin
The hormone alpha-melanocyte stimulating hormone is made when the body is exposed to sunlight and is responsible for the development of the pigment melanin. Research is being done to create stable artificial forms of the hormone. A promising candidate, melanotan, might be useful in the prevention of skin cancer, by causing tanning without the need for exposure to dangerous levels of UV.
Possible health effects
Recently, there has been increased attention to the possibility of adverse health effects associated with the synthetic compounds in most sunscreens.[13] A study published in April 1992, entitled "Could sunscreens increase melanoma risk?" reported that the greatest increase in melanoma has occurred in those regions where sunscreen use is most prevalent.[14] Although one might believe that this effect is due to sunscreens being used more in regions where people are more exposed to UV light, this is not what is claimed by this study: Melanome incidence correlates strongly with the use of chemical sunscreens independently of the actual UV exposure.[15]
In a May 2006 report, "Nanomaterials, Sunscreens and Cosmetics: Small Ingredients, Big Risks", Friends of the Earth claimed that several types of nanoparticles (like titanium dioxide or zinc oxide) can be harmful to human tissue. Currently, there is no policy requiring mandatory product labelling on products that use these compounds.
Some individuals can have mild to moderate allergic reactions to certain ingredients in sunscreen, particularly the chemical benzophenone, which is also known as phenyl ketone, diphenyl ketone, or benzoylbenzene. It is not clear how much of benzophenone is absorbed into the bloodstream, but trace amounts can be found in urinalysis after use.
Recent studies found that sunscreen generates harmful compounds that promote skin cancer. The three commonly used ultraviolet (UV) filters -- octylmethoxycinnamate, benzophenone 3 and octocrylene -- eventually soak into the deeper layers of the skin after their application, leaving the top skin layers vulnerable to sun damage. UV rays absorbed by the skin can generate harmful compounds called reactive oxygen species (ROS), which can cause skin cancer and premature aging. The researchers found that once the filters in sunscreen soak into the lower layers of skin, the filters react with UV light to create more damaging ROS.[16]
A researcher from the University of Manchester, England, has supported other research findings from Harvard University to say that blocking the sunblock creams can interfere with Vitamin D production and fighting some forms of cancer.[17]
Controversy over Sunscreen Sprays
A number of new studies [18] have started to come out concerning the potentcy of sprays versus lotion form.
References
- ↑ 1.0 1.1 http://www.fda.gov/ohrms/dockets/dailys/00/Sep00/090600/c000573_10_Attachment_F.pdf
- ↑ Diffey B (2001). "When should sunscreen be reapplied?". J Am Acad Dermatol 45 (6): 882-5. PMID 11712033. http://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=pubmed&list_uids=11712033&dopt=Citation.
- ↑ Kerry M. Hanson, Enrico Gratton and Christopher J. Bardeen (2006). "Sunscreen enhancement of UV-induced reactive oxygen species in the skin". Free Radical Biology and Medicine 11. http://dx.doi.org/10.1016/j.freeradbiomed.2006.06.011.
- ↑ Holick M (2004). "Sunlight and vitamin D for bone health and prevention of autoimmune diseases, cancers, and cardiovascular disease". Am J Clin Nutr 80 (6 Suppl): 1678S-88S. PMID 15585788. http://www.ajcn.org/cgi/content/full/80/6/1678S?maxtoshow=&HITS=10&hits=10&RESULTFORMAT=1&author1=holick+mf&andorexacttitle=and&andorexacttitleabs=and&andorexactfulltext=and&searchid=1&FIRSTINDEX=0&sortspec=relevance&fdate=1/1/2004&tdate=12/31/2004&resourcetype=HWCIT.
- ↑ Holick M (1995). "Environmental factors that influence the cutaneous production of vitamin D". Am J Clin Nutr 61 (3 Suppl): 638S-645S. PMID 7879731.
- ↑ "Dietary Supplement Fact Sheet: Vitamin D". National Institutes of Health. http://dietary-supplements.info.nih.gov/factsheets/vitamind.asp. Retrieved 2006-06-10.
- ↑ Berneburg M, Plettenberg H, Medve-König K, Pfahlberg A, Gers-Barlag H, Gefeller O, Krutmann J (2004). "Induction of the photoaging-associated mitochondrial common deletion in vivo in normal human skin". J Invest Dermatol 122 (5): 1277-83. PMID 15140232.
- ↑ MSN
- ↑ http://www.m-vskintherapy.com/skinhints.html
- ↑ http://www.fda.gov/bbs/topics/ANSWERS/ANS00955.html
- ↑ GDPR Support
- ↑ http://www.optometrics.com/corporate/support/KFDA.html
- ↑ http://www.straight.com/content.cfm?id=18501
- ↑ Garland C, Garland F, Gorham E (1992). "Could sunscreens increase melanoma risk?". Am J Public Health 82 (4): 614-5. PMID 1546792. http://www.pubmedcentral.nih.gov/articlerender.fcgi?tool=pubmed&pubmedid=1546792.
- ↑ Hans R. Larsen, Sunscreens and Cancer, Int. J. Alternative and Complementary Med., 12, 17 (1994)
- ↑ http://www.newstarget.com/020237.html
- ↑ Skin Cancer: Prevention and Early Detection
- ↑ http://www.usc.edu/CSSF/Current/Projects/J1135.pdf
See also
- Slip-Slop-Slap - famous Australian sun safety advertising jingle
- "Wear Sunscreen" - a column by Mary Schmich in the form of a speech that became a music single and then made into a music video that became viral on the internet
- Indoor tanning lotion
- Sun protective clothing
External links
- FDA monograph on sunscreen
- FDA monograph on dosing, mechanism of action, and photodegradation of sunscreen (PDF file)
- Sunscreen protection calculator
- Sun Safety for Babies and Children University of Florida/IFAS Extension Department of Family, Youth and Community Sciences
- Article on UV absorbers not yet approved by the FDA